Vascular Surgery for ED: When Circulation Is the Root Cause
Erectile dysfunction (ED) affects millions of men worldwide, with estimates suggesting that over 30 million men in the United States alone experience this condition. While medications like PDE5 inhibitors (Viagra, Cialis) have revolutionized treatment, they primarily address symptoms rather than underlying causes. For many men, particularly those with poor response to medications, vascular issues may be at the root of their erectile difficulties.
Vascular-related ED, or vasculogenic ED, accounts for up to 70% of organic ED cases. When blood flow problems are the primary cause, vascular surgery may offer a potential solution. This article explores the relationship between vascular health and erectile function, surgical options for treating vascular ED, and what patients should know when considering these procedures.
Understanding Vascular Causes of Erectile Dysfunction
Before discussing surgical interventions, it’s essential to understand how vascular issues contribute to erectile dysfunction.
The Vascular Mechanics of Erection
An erection is fundamentally a vascular event. During sexual arousal, neural signals trigger the release of nitric oxide in the penis, causing relaxation of smooth muscles in the arteries and erectile tissues. This relaxation allows increased arterial blood flow into the corpora cavernosa (erectile chambers), while simultaneously compressing the veins that normally drain blood from these chambers—a process known as the veno-occlusive mechanism.
Dr. Jonathan Clavell, a urologist specializing in men’s sexual health, explains: “A healthy erection requires three key vascular components: adequate arterial inflow, proper expansion of the erectile tissues, and effective venous occlusion to trap blood within the penis. Problems with any of these components can lead to erectile dysfunction.”
Two Primary Vascular Causes of ED
Vascular ED typically falls into two main categories:
1. Arterial Insufficiency (Arteriogenic ED)
This occurs when the arteries supplying blood to the penis are narrowed or blocked, typically due to:
- Atherosclerosis (plaque buildup in arteries)
- Hypertension (high blood pressure)
- Diabetes-related vascular damage
- Traumatic injury to pelvic or penile arteries
- Smoking-related vascular damage
According to University Hospitals, arterial insufficiency is diagnosed when Doppler ultrasound shows a peak systolic velocity less than 25 cm/s in the cavernosal arteries.
2. Venous Leak (Venogenic ED)
Also known as veno-occlusive dysfunction, venous leak occurs when blood drains too quickly from the penis, preventing the maintenance of an erection. This can result from:
- Structural abnormalities in the tunica albuginea (the fibrous envelope surrounding the erectile tissue)
- Abnormal venous channels that bypass normal occlusion mechanisms
- Degenerative changes in erectile tissues
- Trauma or surgery affecting the penis
- Peyronie’s disease (fibrous scar tissue within the penis)
Dr. Sarah Thompson, vascular surgeon at Mayo Clinic, notes: “Venous leak is often more challenging to treat than arterial insufficiency, as it involves complex mechanisms that maintain blood within the erectile tissues rather than simply delivering blood to the penis.”
Diagnostic Evaluation for Vascular ED
Before considering vascular surgery, a thorough diagnostic evaluation is essential to confirm the vascular etiology and determine the specific type of vascular dysfunction.
Key Diagnostic Tests
- Color Doppler Ultrasonography
- Measures blood flow velocities in penile arteries
- Assesses for arterial stenosis or occlusion
- Evaluates for venous leakage
- Typically performed after an injection of vasodilating medication
- Dynamic Infusion Cavernosometry and Cavernosography (DICC)
- Measures pressure within the erectile chambers
- Assesses the rate of fluid required to maintain an erection
- Visualizes venous leakage sites through X-ray imaging
- Considered the gold standard for diagnosing venous leak
- Selective Pudendal Arteriography
- Provides detailed images of penile arterial anatomy
- Identifies specific locations of arterial blockages
- Essential before arterial reconstruction surgery
- Typically reserved for younger patients considering revascularization
- Additional Evaluations
- Hormonal assessment (testosterone, prolactin)
- Nocturnal penile tumescence testing
- Psychological evaluation
- Assessment of cardiovascular risk factors
Vascular Surgical Options for ED
Several surgical approaches exist for treating vascular ED, with the appropriate choice depending on the specific vascular issue and patient characteristics.
1. Penile Revascularization (Arterial Bypass Surgery)
This procedure aims to increase arterial blood flow to the penis by bypassing blocked arteries.
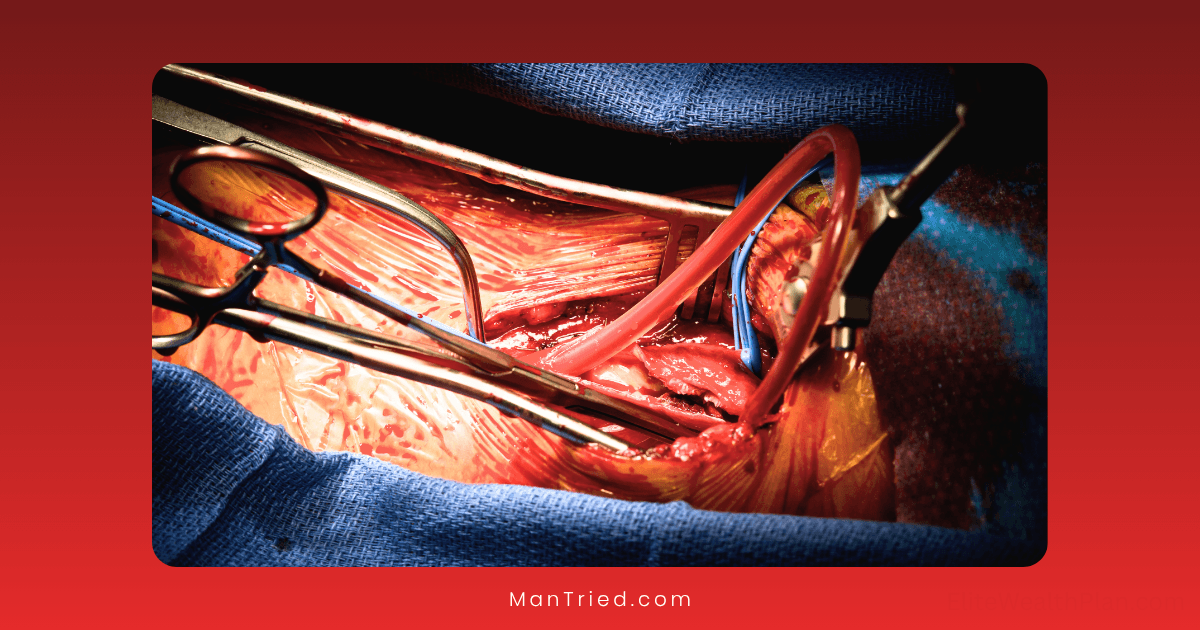
Procedure Details
- An artery (typically the inferior epigastric artery from the abdomen) is harvested
- The donor artery is connected to the dorsal artery or deep dorsal vein of the penis
- The procedure creates a new route for blood to flow into the erectile tissues
- Surgery typically takes 4-6 hours under general anesthesia
- Usually requires one night of hospitalization
According to the Sexual Medicine Society of North America, the most common approach is the Furlow-Fisher technique, which anastomoses the inferior epigastric artery to the dorsal artery of the penis.
Ideal Candidates
Penile revascularization is most appropriate for:
- Younger men (typically under 55)
- Isolated arterial blockage, usually from trauma
- No significant venous leak
- No widespread vascular disease
- No significant risk factors like diabetes or smoking
Outcomes and Success Rates
Research published in the National Library of Medicine indicates that:
- Approximately 50-70% of carefully selected patients report improved erections
- Success rates decline significantly after 5 years
- Results are better in traumatic arterial injuries than atherosclerotic disease
- Younger patients have better outcomes than older patients
2. Venous Ligation Surgery
This procedure aims to correct venous leak by tying off veins that drain blood too quickly from the penis.
Procedure Types
Several approaches exist:
- Dorsal Penile Vein Ligation (DPVL): Ligating the superficial and deep dorsal veins
- Crural Ligation: Addressing leakage from the crura (base) of the penis
- Penile Venous Stripping (PVS): More extensive removal of leaking veins
Procedure Details
- Typically performed under general anesthesia
- May involve a circumferential incision at the base of the penis
- Identification and ligation of leaking veins
- Surgery usually takes 1-3 hours
- Often performed as outpatient surgery
Candidacy and Considerations
Venous surgery is generally considered for:
- Men with documented venous leak on diagnostic testing
- Failure of medical therapy
- Relatively young age (typically under 50)
- No significant arterial disease
However, the American Urological Association generally does not recommend venous ligation due to poor long-term results and potential complications.
Outcomes and Controversy
Venous surgery has shown mixed results:
- Initial success rates of 60-80% have been reported
- Long-term success rates drop significantly, often below 30% after 5 years
- Complications can include penile numbness, deformity, and skin necrosis
- Modern techniques may offer better outcomes than older approaches
Dr. Michael Golowa notes on his clinical website that newer, less invasive approaches like venous embolization may offer better risk-benefit profiles than traditional venous ligation.
3. Venous Embolization
A newer, minimally invasive alternative to venous ligation surgery.
Procedure Details
- Performed under local anesthesia with sedation
- A catheter is inserted through a small incision, typically in the groin
- The catheter is guided to the leaking veins using X-ray guidance
- Medical-grade glue or coils are deployed to block the abnormal veins
- Typically takes 1-2 hours and is performed as an outpatient procedure
Advantages Over Traditional Surgery
- Minimally invasive with smaller incisions
- Lower risk of nerve damage or penile deformity
- Shorter recovery time
- Can be repeated if necessary
Early Results and Considerations
While still considered investigational by some:
- Early studies show 70-80% improvement in erectile function
- Long-term data is still limited
- Not widely available at all medical centers
- May not be covered by insurance
Risks and Complications of Vascular Surgery for ED
All surgical interventions carry risks, and vascular surgeries for ED are no exception.
General Surgical Risks
- Bleeding and hematoma formation
- Infection at surgical sites
- Adverse reactions to anesthesia
- Thrombosis (blood clots)
- Temporary or permanent numbness
Procedure-Specific Complications
For Arterial Revascularization:
- Donor site complications (abdominal wall weakness)
- Graft thrombosis or occlusion
- Priapism (prolonged, painful erection)
- Penile shortening
- Glans hyperemia (excessive blood flow to the glans penis)
For Venous Surgeries:
- Penile deformity or curvature
- Persistent or worsening ED
- Penile skin necrosis
- Permanent sensory loss
- Painful scarring
Alternative Treatments for Vascular ED
Given the limitations and risks of vascular surgery, several alternatives should be considered:
Medical Therapies
- PDE5 inhibitors (Viagra, Cialis, etc.) remain first-line therapy
- Intracavernosal injection therapy (Trimix, Bimix) can be effective even with vascular issues
- Vacuum erection devices work independently of vascular status
- Low-intensity shockwave therapy may improve penile blood flow
Penile Prosthesis
For men with severe vascular ED who don’t respond to other treatments, a penile implant may offer the most reliable solution:
- High satisfaction rates (>90%)
- Reliable, on-demand erections
- No effect from underlying vascular disease
- Minimally visible when not in use
Dr. Rafael Carrion, Professor of Urology at USF Health, explains: “For many men with severe vascular ED, especially those with both arterial and venous issues, a penile implant offers the most predictable and satisfying long-term solution.”
Making an Informed Decision
When considering vascular surgery for ED, several factors should guide the decision-making process:
Key Considerations
- Accurate diagnosis: Ensure thorough vascular testing confirms the specific issue
- Age and overall health: Younger, healthier patients generally have better outcomes
- Cause of vascular dysfunction: Traumatic causes have better surgical outcomes than systemic disease
- Surgeon experience: These procedures require specialized expertise
- Realistic expectations: Understand the potential for both success and failure
- Insurance coverage: Many vascular procedures for ED are not covered by insurance
Questions to Ask Your Surgeon
- What is my specific vascular diagnosis?
- Am I an ideal candidate for this procedure based on age and health status?
- What is your experience with this specific procedure?
- What are my chances of success, both short and long-term?
- What alternatives should I consider before surgery?
- What complications have your patients experienced?
Conclusion: Is Vascular Surgery Right for You?
Vascular surgery for erectile dysfunction represents a potential option for carefully selected patients, particularly younger men with traumatic arterial injuries or specific venous leak patterns. However, these procedures come with significant limitations, including variable success rates, potential complications, and limited long-term efficacy.
For most men with vascular ED, a stepwise approach is recommended:
- Trial of oral medications and lifestyle modifications
- Consideration of injection therapy or vacuum devices if oral medications fail
- Evaluation for vascular surgery only in specific cases (young age, traumatic cause)
- Consideration of penile prosthesis if other approaches are unsuccessful
As with any treatment for erectile dysfunction, the decision should be individualized based on the specific cause, patient characteristics, and preferences. A thorough discussion with a urologist specializing in sexual medicine is essential to determine the most appropriate approach for each individual.