Fertility Preservation for Young Men: Options and Considerations
For young men facing medical treatments that may impact fertility, planning for future reproductive options has never been more important. Advances in fertility preservation technologies offer multiple pathways to parenthood, even after undergoing potentially fertility-compromising treatments. Whether you’re facing a cancer diagnosis, preparing for gender-affirming care, or simply want to preserve fertility options for the future, understanding your choices is crucial.
This comprehensive guide explores the options available for male fertility preservation, along with important considerations about costs, success rates, and decision-making factors.
Why Consider Fertility Preservation?
Several situations may prompt young men to consider preserving their fertility:
Medical Treatments That Impact Fertility
Many medical treatments can temporarily or permanently affect male fertility:
- Cancer treatments: Chemotherapy and radiation therapy can damage sperm-producing cells, with the risk varying based on drug types, dosages, and radiation fields.
- Surgery: Procedures involving the reproductive organs, such as radical prostatectomy, can affect ejaculation or sperm production.
- Hormone therapies: Certain medications used for various conditions can impact sperm production.
- Gender-affirming care: Hormonal treatments and surgeries for transgender individuals may affect fertility.
Dr. James Chen, reproductive urologist at University Medical Center, explains: “The good news is that with proper planning, many young men can preserve their fertility before undergoing treatments that might otherwise limit their reproductive options. The key is having these conversations early in the treatment planning process.”
Long-term Planning
Even without immediate medical concerns, some young men choose fertility preservation for future planning:
- Delaying parenthood while focusing on education or career
- Preserving younger, healthier sperm for future use
- Providing reproductive insurance before high-risk occupations or activities
- Peace of mind regarding future family-building options
Fertility Preservation Options for Young Men
Sperm Banking (Semen Cryopreservation)
Sperm banking remains the most established and widely used method of fertility preservation for post-pubertal males.
The Process
- Collection: Sperm is typically collected through masturbation in a private room at a fertility clinic or sperm bank.
- Analysis: The sample is examined to assess sperm count, motility, and morphology.
- Processing: The sample is mixed with a cryoprotectant solution to protect sperm during freezing.
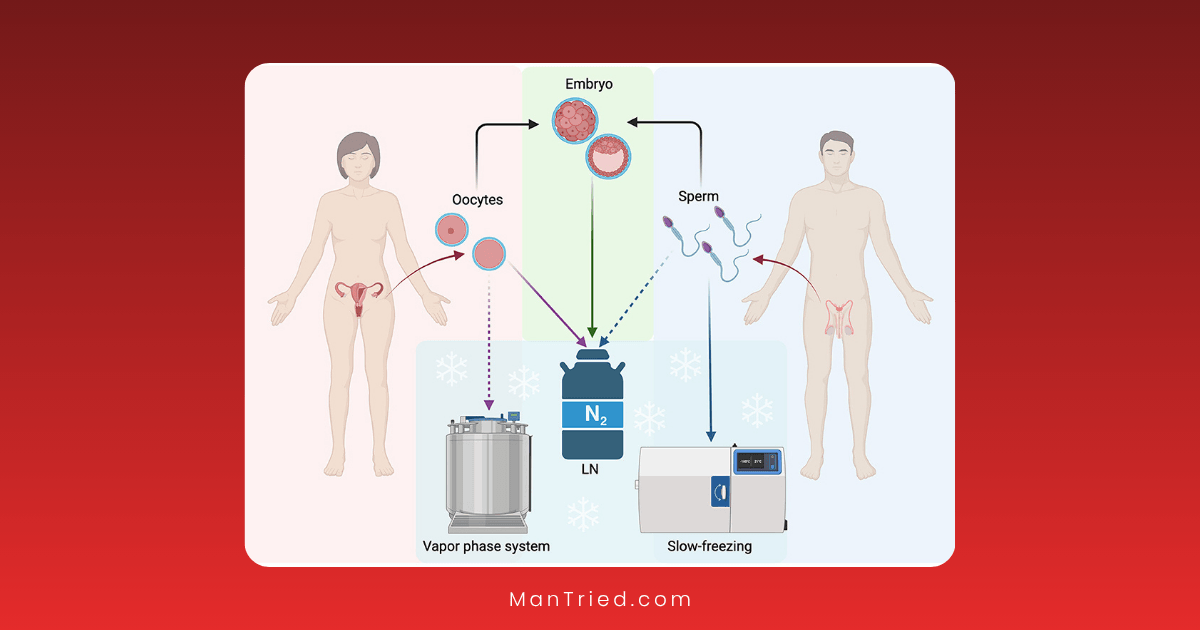
- Freezing: Using controlled-rate freezing or vitrification techniques, the sample is frozen and stored in liquid nitrogen.
- Storage: Samples can be stored indefinitely with proper maintenance.
Success Rates
Sperm banking offers excellent long-term success rates:
- Approximately 50% of sperm survive the freezing and thawing process
- Pregnancy rates using frozen sperm are comparable to those using fresh sperm, depending on the female partner’s fertility and the assisted reproduction method used
- Even samples with lower sperm counts can be successfully used with advanced reproductive techniques like intracytoplasmic sperm injection (ICSI)
“The viability of properly frozen sperm doesn’t decrease over time,” notes fertility specialist Dr. Sarah Williams. “We’ve seen successful pregnancies using sperm that was frozen decades earlier, which offers tremendous peace of mind for young men preserving fertility.”
Timing Considerations
For optimal results:
- Bank sperm before beginning fertility-compromising treatments
- Provide multiple samples when possible (ideally 2-3 samples, a few days apart)
- Allow 2-3 days of abstinence before each collection
Testicular Sperm Extraction (TESE)
For men who cannot produce a semen sample or have no sperm in their ejaculate, surgical sperm retrieval offers an alternative.
The Process
- Surgical procedure: A urologist removes small pieces of testicular tissue through a small incision in the scrotum.
- Laboratory processing: The tissue is examined for viable sperm.
- Cryopreservation: Any found sperm are frozen for future use.
Success Rates
TESE outcomes vary based on individual factors:
- Success rates range from 30-70% for finding viable sperm
- Studies show live sperm present up to 45% of the time in men with no sperm in their ejaculate after cancer treatment
- When combined with ICSI, pregnancy rates are comparable to those using ejaculated sperm
Best Candidates
TESE may be appropriate for:
- Men with non-obstructive azoospermia (absence of sperm in ejaculate)
- Cancer patients who didn’t bank sperm before treatment
- Men with ejaculatory dysfunction
- Those with very low sperm counts in ejaculate
Testicular Tissue Freezing
For prepubertal boys who are not yet producing sperm, testicular tissue freezing offers a potential future option.
The Process
- Surgical biopsy: A small amount of testicular tissue is surgically removed.
- Freezing: The tissue containing spermatogonial stem cells is cryopreserved.
- Future use: The tissue may potentially be reimplanted or matured in the laboratory in the future.
Current Status
This approach is still considered experimental:
- No human live births have been reported using this technique as of 2025
- Animal studies have shown promising results
- Several techniques for using the tissue are under development
“Testicular tissue freezing represents the frontier of fertility preservation for young boys facing cancer treatments,” explains pediatric oncologist Dr. Michael Torres. “While still experimental, it offers hope for the youngest patients who previously had no options for preserving fertility.”
Radiation Shielding
For men undergoing radiation therapy, protective measures can help minimize damage to reproductive organs.
The Process
- Lead shields are strategically placed to protect the testicles during radiation treatments
- Treatment planning aims to minimize radiation exposure to reproductive organs
Effectiveness
The effectiveness depends on:
- The proximity of the treatment area to the testicles
- The total radiation dose
- The success of shielding implementation
Cost and Insurance Considerations
Understanding the financial aspects of fertility preservation is crucial for planning.
Typical Costs
Costs vary by procedure and location:
- Sperm banking: $500-$1,000 for initial analysis and freezing, plus $200-$500 annually for storage
- TESE: $6,000-$16,000 for the procedure
- Testicular tissue freezing: Approximately $2,500 for surgery, plus $300-$500 annually for storage
- Radiation shielding: Typically included in radiation treatment costs
Insurance Coverage
Insurance coverage for fertility preservation has improved but remains inconsistent:
- As of 2025, 22 U.S. states and the District of Columbia have laws mandating some level of insurance coverage for fertility treatments
- 16 states specifically mandate coverage for fertility preservation
- Coverage varies significantly between plans, even in states with mandates
- Only 3 states mandate coverage for non-commercial plans like Medicaid
- Approximately 17.8% of training programs offer insurance coverage for fertility preservation
Financial Assistance Options
Several resources can help manage costs:
- Livestrong Fertility Program: Provides discounted services and medications for cancer patients
- The Samfund: Offers grants for young adult cancer survivors
- Team Maggie: Provides financial support for fertility preservation for cancer patients
- Hospital financial assistance programs: Many institutions offer sliding-scale fees or payment plans
- Compassionate care programs: Some pharmaceutical companies provide medications at reduced costs
Dr. Williams advises: “Don’t assume fertility preservation is financially out of reach. Many patients are surprised to learn about the assistance programs available, especially for those with cancer diagnoses. Always ask about financial resources when discussing fertility preservation options.”
Decision-Making Factors
Several factors should influence the choice of fertility preservation method:
Medical Considerations
- Urgency of medical treatment: Some cancer treatments cannot be delayed, limiting preservation options
- Type and dose of treatment: Different treatments carry varying risks to fertility
- Current fertility status: Pre-existing fertility issues may influence the recommended approach
- Age and pubertal status: Determines which preservation options are available
Personal Factors
- Desire for future biological children: The strength of this desire affects the importance of preservation
- Relationship status: Current partnership status may influence decisions but shouldn’t limit options
- Religious or ethical considerations: Personal beliefs may impact acceptable preservation methods
- Comfort with various procedures: Psychological comfort with different methods varies by individual
Practical Considerations
- Cost and insurance coverage: Financial realities may limit options
- Geographic access to services: Not all preservation methods are available in all locations
- Time constraints: Some methods require multiple appointments or recovery time
- Long-term storage plans: Consider where and how long samples will be stored
Special Considerations for Different Populations
Adolescents and Young Adults with Cancer
Young cancer patients face unique challenges:
- Only about 30% report having fertility preservation discussed by their oncologist
- Parental involvement may complicate decision-making for minors
- Urgent treatment needs may limit time for preservation
- Long-term survivorship planning is essential
Research indicates that approximately 35,000 new cases of childhood and adolescent cancer are reported annually in Europe, with long-term survival expected in about 80% of these young patients. This highlights the growing importance of fertility preservation discussions.
Transgender Men
For transgender men considering hormonal or surgical transition:
- Fertility preservation ideally occurs before starting testosterone therapy
- Options include oocyte (egg) or embryo freezing
- Temporary cessation of hormone therapy may be required for preservation
- Psychological support during the process is particularly important
Men with Non-Malignant Conditions
Several non-cancer conditions may require treatments affecting fertility:
- Autoimmune disorders requiring immunosuppressive therapy
- Sickle cell disease or thalassemia requiring bone marrow transplant
- Conditions requiring long-term medication with fertility impacts
- Genetic conditions with fertility implications
The Process: What to Expect
Understanding the typical process helps reduce anxiety and ensures proper preparation.
Initial Consultation
The fertility preservation journey typically begins with a consultation that includes:
- Discussion of medical history and future treatment plans
- Assessment of current fertility status when possible
- Explanation of available options
- Review of costs and insurance coverage
- Addressing questions and concerns
Pre-Preservation Preparation
Before preservation procedures:
- Follow any abstinence guidelines provided (typically 2-3 days for sperm banking)
- Complete required consent forms and legal documentation
- Make financial arrangements
- Consider genetic testing if relevant to your situation
- Arrange support for appointments if needed
After Preservation
Once preservation is complete:
- Confirm storage arrangements and understand annual fees
- Keep contact information updated with the storage facility
- Consider legal aspects of using preserved materials in the future
- Focus on medical treatment with reduced fertility anxiety
Future Utilization of Preserved Materials
Understanding how preserved sperm or tissue might be used in the future can inform current decisions.
Assisted Reproductive Technologies
Preserved sperm can be used with various fertility treatments:
- Intrauterine insemination (IUI): Processed sperm is placed directly into the uterus during ovulation
- In vitro fertilization (IVF): Eggs are fertilized with sperm in a laboratory setting
- Intracytoplasmic sperm injection (ICSI): A single sperm is injected directly into an egg
- Gestational surrogacy: Another woman carries the pregnancy if the intended mother cannot
Success Rates with Preserved Sperm
Success rates depend on multiple factors:
- The quality and quantity of preserved sperm
- The age and fertility status of the female partner
- The chosen assisted reproductive technology
- The expertise of the fertility clinic
Current data suggests that pregnancy rates using frozen sperm are comparable to those using fresh sperm when appropriate techniques are used.
Emotional and Psychological Aspects
The fertility preservation journey involves significant emotional components that shouldn’t be overlooked.
Common Emotional Responses
Many young men experience:
- Anxiety about future fertility
- Grief over potential fertility loss
- Embarrassment about the preservation process
- Worry about the financial burden
- Uncertainty about future family planning
- Relief after completing preservation
Support Resources
Several resources can provide emotional support:
- Mental health professionals specializing in reproductive issues
- Peer support groups for those undergoing similar experiences
- Online communities focused on fertility preservation
- Patient navigators at cancer centers or fertility clinics
“The psychological impact of facing potential fertility loss shouldn’t be underestimated,” notes psychologist Dr. Elena Rodriguez, who specializes in reproductive health issues. “Having open conversations and accessing appropriate support can make a tremendous difference in navigating this challenging experience.”
Emerging Technologies and Future Directions
The field of male fertility preservation continues to evolve rapidly.
Research Developments
Promising areas of research include:
- In vitro spermatogenesis: Laboratory maturation of sperm from testicular stem cells
- Artificial gametes: Creating sperm-like cells from other cell types
- Testicular tissue grafting: Transplanting preserved tissue to produce sperm
- Bioengineered testicles: Creating functional testicular tissue in the laboratory
Experimental Approaches
Several experimental approaches show promise:
- Spermatogonial stem cell transplantation: Reintroducing preserved stem cells to restore sperm production
- Hormone therapy protection: Medications that may protect fertility during cancer treatment
- Testicular tissue reimplantation: Returning cryopreserved tissue to restore function
Conclusion: Taking Action
Fertility preservation represents an important aspect of comprehensive healthcare for young men facing fertility-threatening conditions or treatments. By understanding the available options, associated costs, and decision-making factors, young men can make informed choices about their reproductive futures.
The most important steps are:
- Start the conversation early: Discuss fertility preservation with healthcare providers as soon as possible
- Understand all options: Review the preservation methods appropriate for your situation
- Consider future family planning: Think about how many children you might want in the future
- Explore financial resources: Investigate insurance coverage and assistance programs
- Seek emotional support: Acknowledge the psychological impact and access appropriate resources
As Dr. Chen emphasizes: “The biggest regret we see is not from men who preserved fertility they didn’t end up needing, but from those who didn’t preserve when they had the chance. When in doubt, having the option is invaluable for future peace of mind.”
By taking proactive steps toward fertility preservation, young men can maintain reproductive options regardless of medical challenges, providing hope and possibilities for future family building.
Have you considered fertility preservation or have questions about the process? Share your thoughts or questions in the comments below.






