Bioidentical Hormones: The Future of Testosterone Replacement?

In the evolving landscape of men’s health, few topics generate as much interest—and controversy—as bioidentical hormone replacement therapy (BHRT). With testosterone levels in American men declining at approximately 1% per year after age 30, and nearly 40% of men over 45 experiencing symptoms of low testosterone, the search for optimal hormone replacement solutions continues to intensify.
Bioidentical hormones are often marketed as a more “natural” approach to testosterone replacement therapy (TRT). But do they truly represent the future of hormone therapy for men, or is the hype outpacing the evidence? This comprehensive guide examines the science, benefits, risks, and future prospects of bioidentical testosterone therapy.
Understanding Bioidentical Hormones
Before evaluating their potential as the future of TRT, it’s essential to understand what bioidentical hormones actually are:
What Makes a Hormone “Bioidentical”?
The term “bioidentical” refers to hormones that are chemically identical in structure to those naturally produced by the human body. For testosterone, this means the molecule has the exact same chemical structure as the testosterone produced in your testes.
This differs from some synthetic hormones that may have a slightly altered chemical structure. However, it’s important to note that even “bioidentical” hormones used in therapy are still synthesized in laboratories—they don’t come directly from natural sources.
FDA-Approved vs. Compounded Bioidentical Hormones
A critical distinction that’s often overlooked in discussions about bioidentical hormones:
FDA-Approved Bioidentical Hormones:
- Manufactured by pharmaceutical companies under strict quality control
- Tested for safety and efficacy in clinical trials
- Consistent dosing and potency
- Examples include AndroGel, Testim, and Androderm
Compounded Bioidentical Hormones:
- Custom-made by compounding pharmacies
- Not FDA-approved for safety and efficacy
- May vary in quality and consistency
- Often marketed as “personalized” to the individual
According to the National Academies of Sciences, between 1 and 2.5 million Americans use compounded bioidentical hormone therapies, with 26-33 million prescriptions filled annually.
The Science: Evidence for Bioidentical Testosterone
The marketing of bioidentical testosterone often outpaces the scientific evidence. Here’s what the research actually shows:
Clinical Evidence for FDA-Approved Bioidentical Testosterone
FDA-approved bioidentical testosterone products have been studied in clinical trials and shown to:
- Increase serum testosterone levels to the normal range
- Improve sexual function in men with hypogonadism
- Increase lean body mass
- Improve bone mineral density
- Enhance mood and energy levels in men with documented low testosterone
These benefits are similar to those seen with conventional testosterone replacement therapy, as both contain the same active molecule.
Evidence for Compounded Bioidentical Testosterone
The evidence for compounded bioidentical testosterone is much more limited:
- Few randomized controlled trials comparing compounded products to FDA-approved options
- Limited data on long-term safety
- Concerns about dosing consistency and quality control
- No comprehensive clinical outcomes trials
According to the Endocrine Society, “there is little to no scientific evidence supporting claims that compounded bioidentical hormone therapy is safer or more effective than FDA-approved hormone therapies.”
Delivery Methods and Innovations
One area where bioidentical testosterone therapy has seen significant innovation is in delivery methods:
Current Bioidentical Testosterone Delivery Options
1. Transdermal Applications
- Gels and creams: Applied daily to the skin, providing steady hormone levels
- Patches: Deliver consistent doses through the skin over 24 hours
- Advanced formulations: Newer products feature improved absorption and reduced transfer risk
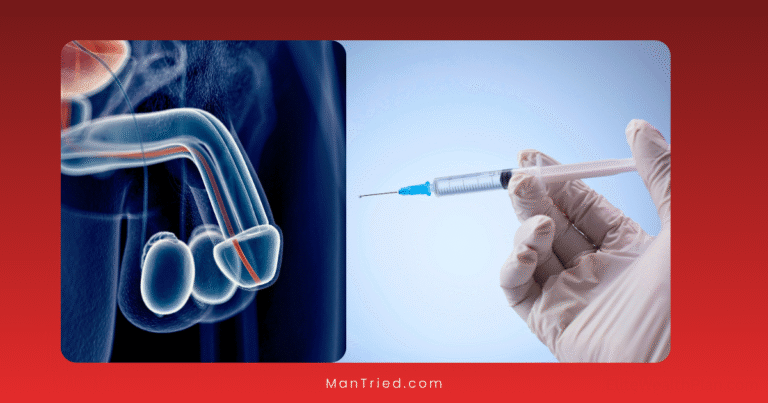
2. Injectable Bioidentical Testosterone
- Testosterone cypionate and enanthate: FDA-approved bioidentical esters
- Microdosing protocols: Smaller, more frequent injections for stable levels
- Long-acting formulations: Extended-release options requiring less frequent administration
3. Implantable Pellets
- Small pellets inserted under the skin
- Provide sustained release over 3-6 months
- Bioidentical testosterone pellets are increasingly popular for their convenience and consistent delivery
4. Newer Delivery Systems
- Buccal adhesives: Applied to the gums for mucosal absorption
- Nasal gels: Rapid absorption through nasal mucosa
- Oral testosterone undecanoate: Lymphatic absorption with reduced liver impact
Personalization Approaches
A key selling point of bioidentical hormone therapy is personalization:
Conventional Personalization:
- Adjusting standard FDA-approved products based on blood tests and symptoms
- Titrating dose and frequency to achieve optimal levels
- Monitoring and adjusting based on response
Advanced Personalization Claims:
- Customized hormone formulations based on individual hormone profiles
- Combination with other hormones (DHEA, pregnenolone, etc.)
- Integration with lifestyle, nutrition, and supplementation
While personalization is appealing, the Endocrine Society notes that “careful control of hormone therapy regimens is difficult even with FDA-approved formulations, due to the challenges in accurately regulating blood hormone levels.”
Potential Benefits of Bioidentical Testosterone
Proponents of bioidentical testosterone therapy cite several potential advantages:
Theoretical Advantages
- Molecular recognition: The identical structure may be more readily recognized by the body’s receptors
- Metabolic pathways: Natural metabolic breakdown pathways may process bioidentical hormones more efficiently
- Reduced side effects: Some practitioners claim fewer side effects due to the identical structure
Reported Benefits from Clinical Practice
Men using bioidentical testosterone therapy often report:
- Increased energy and vitality
- Enhanced libido and sexual function
- Improved body composition (more muscle, less fat)
- Better mood and cognitive function
- Increased motivation and drive
It’s important to note that these benefits are similar to those reported with any effective testosterone replacement therapy, whether bioidentical or not.
Risks and Considerations
Despite marketing claims about superior safety, bioidentical testosterone carries many of the same risks as conventional TRT:
Common Risks of All Testosterone Therapy
- Erythrocytosis: Increased red blood cell production
- Testicular atrophy: Shrinkage of the testicles and reduced sperm production
- Acne and oily skin: Due to androgenic effects
- Sleep apnea: Potential worsening in predisposed individuals
- Cardiovascular considerations: Ongoing research into potential risks
Specific Concerns with Compounded Bioidentical Testosterone
- Dosing inconsistency: Potential variability in hormone content
- Quality control issues: Less rigorous manufacturing standards
- Monitoring challenges: Difficulty establishing appropriate testing protocols
- Pellet complications: Up to 10% extrusion rate and risks of infection or bleeding
The Cleveland Clinic emphasizes that “many healthcare providers claim compounded bioidentical hormones are safer than traditional hormone therapy, but there is no large research evidence to support this.”
Regulatory Landscape and Future Directions
The regulatory environment around bioidentical hormones continues to evolve:
Current Regulatory Status
- FDA-approved bioidentical testosterone products are regulated like any prescription medication
- Compounded bioidentical hormones fall into a regulatory gray area
- The FDA has expressed concerns about marketing claims for compounded products
- Professional medical organizations generally recommend FDA-approved options when available
Emerging Trends for 2025 and Beyond
Several trends are likely to shape the future of bioidentical testosterone therapy:
1. Advanced Diagnostics
- AI-driven diagnostic tools analyzing genetic, metabolic, and lifestyle factors
- More comprehensive hormone testing beyond just testosterone
- Wearable devices for continuous monitoring
2. Delivery Innovations
- Smart delivery systems with programmable release patterns
- Biodegradable long-term implants
- Nanotechnology-enhanced formulations for improved absorption
3. Integrative Approaches
- Combination with peptide therapies
- Metabolic optimization protocols
- Microbiome-based approaches to hormone regulation
4. Regulatory Evolution
- Increased oversight of compounding pharmacies
- More standardized protocols for bioidentical hormone therapy
- Potential new FDA-approved bioidentical options
Making Informed Decisions: Bioidentical vs. Conventional TRT
If you’re considering testosterone therapy, how should you evaluate bioidentical options?
Key Questions to Ask Your Healthcare Provider
- Is my testosterone truly low based on comprehensive testing?
- What are the FDA-approved bioidentical options for my situation?
- If considering compounded formulations, what evidence supports their use?
- How will we monitor effectiveness and safety?
- What is the total cost comparison between options?
Finding the Right Provider
The provider you choose significantly impacts your experience with any form of TRT:
- Endocrinologists: Specialists in hormone disorders with extensive training
- Urologists: Experts in male reproductive health
- Anti-aging/Functional Medicine: Often focus on bioidentical hormones but vary in training
- Primary Care: May manage straightforward TRT but refer complex cases
Look for providers who:
- Conduct comprehensive testing before prescribing
- Discuss all available options, not just bioidentical
- Have established monitoring protocols
- Are transparent about risks and benefits
- Base recommendations on scientific evidence
The Bottom Line: Are Bioidentical Hormones the Future of TRT?
Bioidentical testosterone therapy represents an important option in the treatment landscape for men with hypogonadism, but claims of superiority over conventional TRT remain largely unsubstantiated by high-quality evidence.
The future likely involves:
- Continued use of FDA-approved bioidentical testosterone products
- More rigorous research on compounded formulations
- Advanced delivery systems for improved convenience and consistency
- Better personalization based on genetic and metabolic factors
- Integration with lifestyle and other therapeutic approaches
For most men, the best approach is to:
- Confirm low testosterone with proper testing
- Start with FDA-approved options (many of which are already bioidentical)
- Monitor response and adjust as needed
- Consider compounded options only when standard treatments are insufficient
While the marketing of bioidentical hormones often promises revolutionary benefits, the science suggests a more measured view: they are a valuable tool in the hormone replacement arsenal, but not a magical solution that transcends the basic principles of endocrinology and medicine.
Have you tried bioidentical testosterone therapy? Share your experiences in the comments below.