Living and Loving with Herpes: Management and Disclosure

Receiving a herpes diagnosis can feel overwhelming. In a culture where sexually transmitted infections (STIs) are often stigmatized, herpes in particular seems to carry a disproportionate psychological burden. Yet the reality is far less dire than many initially fear. With proper management, open communication, and self-compassion, people with herpes lead fulfilling romantic and sexual lives every day.
This comprehensive guide will walk you through the practical aspects of living with herpes—from medical management to relationship navigation—with evidence-based information and compassionate advice.
Understanding Herpes: The Facts Beyond the Stigma
Before diving into management and disclosure, it’s important to understand what we’re actually dealing with:
Prevalence: You Are Far From Alone
According to the Centers for Disease Control and Prevention (CDC), herpes is extremely common:
- HSV-1 (typically associated with oral herpes but can cause genital herpes): Affects approximately 67% of people under 50 globally
- HSV-2 (typically causes genital herpes): Affects about 1 in 8 Americans aged 14-49
Dr. Jenelle Marie Pierce, Executive Director of The STI Project, notes: “The prevalence of herpes means that most sexually active adults will encounter it at some point, whether they realize it or not.”
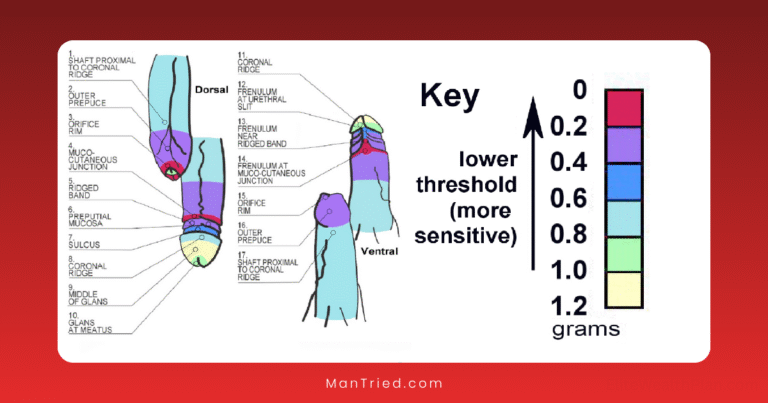
Transmission Basics
Understanding transmission helps both management and partner conversations:
- Herpes spreads through skin-to-skin contact with infected areas
- Transmission can occur even without visible symptoms (asymptomatic shedding)
- The risk is highest during outbreaks
- Condoms reduce transmission risk by approximately 50%
- Daily antiviral medication can reduce transmission risk by up to 90%
Medical Management: Controlling Symptoms and Reducing Transmission
Effective medical management serves two purposes: reducing your discomfort and lowering the risk of transmitting the virus to partners.
Antiviral Medications
Three prescription medications are FDA-approved for herpes management:
- Acyclovir (Zovirax): The original antiviral, typically taken multiple times daily
- Valacyclovir (Valtrex): A newer formulation that requires fewer daily doses
- Famciclovir (Famvir): Similar to valacyclovir in dosing convenience
These medications can be used in two ways:
- Episodic therapy: Taking medication at the first sign of an outbreak to reduce severity and duration
- Suppressive therapy: Taking medication daily to reduce outbreak frequency and asymptomatic shedding
According to a study published in the Journal of Infectious Diseases, daily suppressive therapy can reduce asymptomatic viral shedding by up to 80% and decrease transmission risk by about 50%.
Dr. Christine Johnston, a herpes researcher at the University of Washington, explains: “For people in relationships where one partner has herpes and the other doesn’t, combining daily suppressive therapy with condoms provides the best protection currently available.”
Identifying and Managing Triggers
Many people with herpes identify specific factors that trigger outbreaks:
- Stress (physical or emotional)
- Menstruation
- Illness or fever
- Sun exposure
- Friction from clothing or sexual activity
- Certain foods (particularly those high in arginine like chocolate, nuts, and seeds)
Keeping a symptom journal can help identify your personal triggers. The American Sexual Health Association recommends tracking potential triggers, outbreak timing, and severity to recognize patterns.
Supporting Your Immune System
A healthy immune system helps control the virus:
- Adequate sleep (7-9 hours for most adults)
- Regular physical activity
- Balanced nutrition
- Stress management techniques (meditation, yoga, deep breathing)
- Limited alcohol consumption
The Psychological Impact: Moving Beyond Shame
The psychological burden of herpes often exceeds its physical impact. Research published in BMC Public Health found that a herpes diagnosis can trigger feelings of shame, fear of rejection, and concerns about future relationships.
Reframing Your Perspective
Dr. Sheila Loanzon, author of “Yes, I Have Herpes,” suggests these reframing strategies:
- Separate facts from feelings: Herpes is a common skin condition, not a reflection of your character or worth
- Challenge catastrophic thinking: Most relationships continue successfully after disclosure
- Focus on education: Understanding the virus reduces fear for both you and potential partners
- Connect with others: Support groups (online or in-person) provide perspective and community
Professional Support
If herpes-related anxiety or depression is interfering with your quality of life, consider professional help:
- Therapists: Look for professionals with experience in sexual health issues or chronic conditions
- Support groups: Organizations like the National Herpes Resource Center offer resources
- Online communities: Forums like r/Herpes provide peer support
Disclosure: The Art of Difficult Conversations
Perhaps the most challenging aspect of living with herpes is telling potential partners. Yet research consistently shows that thoughtful disclosure builds trust and actually reduces transmission rates.
When to Disclose
Timing matters. According to sexual health experts:
- Too early (first date) may create unnecessary pressure
- Too late (after sexual intimacy) violates trust and consent
- The sweet spot: When mutual interest is clear but before sexual activity begins
Dr. Ina Park, author of “Strange Bedfellows,” recommends: “Disclose when you’re starting to feel a connection but before clothes come off. This gives your partner time to process without feeling pressured to make an immediate decision.”
How to Disclose: Conversation Frameworks
While there’s no perfect script, these frameworks provide a starting point:
The Direct Approach
“Before we go further, I want to share something important. I have herpes. I take medication to manage it and am happy to answer any questions you might have about what that means for us.”
The Educational Approach
“I want to talk about sexual health before we become intimate. I have herpes, which is actually very common—about 1 in 6 adults has it. I manage it with medication, and with some basic precautions, the risk of transmission is quite low. I’d be happy to share more information or answer any questions.”
The Contextual Approach
“I really enjoy our connection and see potential for intimacy. Before that happens, I want you to know that I have herpes. I’ve had it for [time period], and I’ve learned how to manage it effectively. I understand if you need time to think about this, and I’m open to discussing any concerns.”
Preparing for Questions
Partners typically ask similar questions. Having answers ready helps the conversation flow:
- How did you get it? (Note: You’re not obligated to share this if you’re uncomfortable)
- How contagious is it?
- How do you manage it?
- What precautions should we take?
- How often do you have outbreaks?
- Can you still have children? (Yes, with proper medical management)
Handling Reactions
Responses vary widely. Be prepared for:
- Acceptance: Many people respond with understanding
- Questions: Provide factual, non-dramatic answers
- Time to process: Respect their need to research and consider
- Rejection: While painful, remember this reflects their limitations, not yours
A survey by the Herpes Resource Center found that 79% of people with herpes reported at least one positive disclosure experience, with many partners appreciating the honesty and responsibility shown.
Navigating Intimate Relationships
Once disclosure is behind you, the focus shifts to building and maintaining healthy relationships.
Safer Sex Practices
For couples where one partner has herpes and the other doesn’t (discordant couples):
- Barrier methods: Condoms and dental dams reduce (but don’t eliminate) transmission risk
- Medication: Daily suppressive therapy significantly reduces viral shedding
- Outbreak awareness: Avoiding sexual contact during prodrome (pre-outbreak symptoms) and active outbreaks
- Communication: Ongoing dialogue about symptoms and comfort levels
When Both Partners Have Herpes
If both partners have the same type of herpes (both HSV-1 or both HSV-2), transmission concerns are minimal. However, it’s still important to:
- Avoid sexual contact during outbreaks to prevent aggravating symptoms
- Communicate about symptoms and respect each other’s comfort levels
- Continue medical management if outbreaks are frequent or severe
Long-Term Relationship Considerations
As relationships mature, herpes often becomes less central to the partnership:
- Evolving risk tolerance: Some couples choose to modify precautions over time
- Shared decision-making: Regularly revisit and adjust your approach together
- Family planning: Work with healthcare providers to minimize transmission risk during conception and pregnancy
Dr. Terri Warren, herpes specialist and author, notes: “In my 33 years of practice, I’ve seen countless couples navigate herpes successfully. Over time, it typically becomes just one small aspect of their relationship rather than a defining feature.”
Special Situations and Considerations
Dating Apps and Online Dating
Some people choose to disclose their status in dating profiles. Pros and cons include:
Pros:
- Filters out incompatible matches early
- Reduces anxiety about when to disclose
- Connects you with open-minded individuals
Cons:
- Potential privacy concerns
- May lead to unnecessary rejection before connection is established
- Defines you primarily by your herpes status
Alternative approaches include using herpes-specific dating platforms like Positive Singles or MPWH (Meet People With Herpes).
Pregnancy and Herpes
With proper medical management, people with herpes safely have children every day:
- Pre-conception: Discuss suppressive therapy with your healthcare provider
- During pregnancy: Continued monitoring and potentially suppressive therapy in the third trimester
- Delivery considerations: C-section may be recommended if active lesions are present during labor
According to the American College of Obstetricians and Gynecologists, the risk of neonatal herpes is very low (less than 1%) when appropriate precautions are taken.
Self-Advocacy in Healthcare
Unfortunately, not all healthcare providers approach herpes with updated knowledge and sensitivity. Advocating for yourself includes:
- Requesting specific tests: Standard STI panels often don’t include herpes testing
- Discussing suppressive therapy options: If your provider seems reluctant, ask for their reasoning
- Seeking second opinions: If you feel dismissed or stigmatized
- Asking for resources: Many providers can recommend support groups or counseling
The Future of Herpes Management
Research continues to advance our understanding and treatment of herpes:
- Vaccine research: Several therapeutic and preventive vaccines are in development
- New antivirals: Researchers are working on more effective medications
- Testing improvements: More accurate and accessible testing methods are evolving
While not yet available, these advances offer hope for even better management options in the future.
Conclusion: Thriving Beyond the Diagnosis
A herpes diagnosis may temporarily feel like a defining moment, but for most people, it ultimately becomes a manageable aspect of health rather than a life-altering condition.
Ella Dawson, a prominent herpes activist, puts it this way: “Having herpes has not prevented me from dating, having sex, or building meaningful relationships. If anything, it’s helped me develop better communication skills and connect more authentically with partners.”
By combining effective medical management, thoughtful disclosure approaches, and self-compassion, you can create a fulfilling romantic and sexual life that isn’t defined or limited by herpes. The initial adjustment period may be challenging, but countless people before you have navigated this path successfully—and you can too.