The Erection Process Explained: Vascular, Neurological, and Hormonal Factors

The human erection is a remarkable feat of biological engineering—a complex interplay of vascular, neurological, and hormonal systems working in precise coordination. While often taken for granted when functioning properly, this intricate process reveals the sophisticated design of human physiology.
Despite its fundamental role in human reproduction and sexual pleasure, the science behind erections remains poorly understood by many. This comprehensive guide explains the physiological mechanisms that transform the flaccid penis into its erect state, exploring the vascular, neurological, and hormonal factors that make this transformation possible.
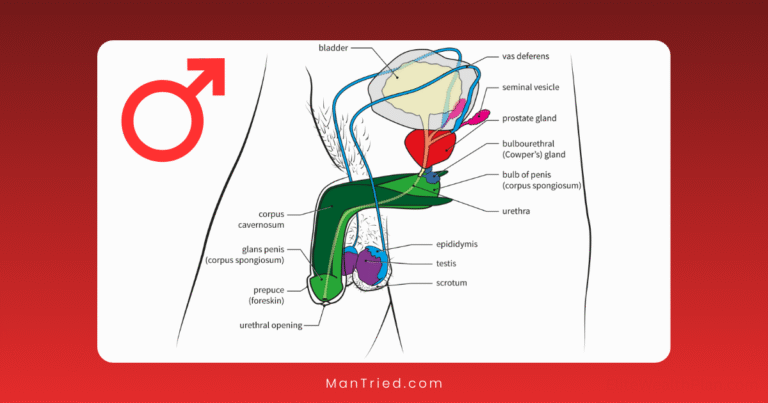
The Anatomy Behind the Action
Before diving into the process itself, it’s important to understand the key anatomical structures involved in erections.
The Three Chambers
The penis contains three cylindrical chambers:
- Two corpora cavernosa: These parallel chambers run along the top of the penis and are the primary erectile tissues. According to NCBI, these chambers “are surrounded by the tunica albuginea, which provides structural support and helps maintain rigidity during an erection.”
- One corpus spongiosum: This chamber runs along the underside of the penis, surrounds the urethra, and forms the glans (head) of the penis. It fills with blood during erection but at lower pressure than the corpora cavernosa.
Vascular Supply
The blood supply to the penis is primarily provided by:
- Internal pudendal artery: A branch of the internal iliac artery
- Dorsal artery: Supplies the skin, glans, and distal urethra
- Cavernous arteries: Supply the erectile tissue of the corpora cavernosa
- Bulbourethral artery: Supplies the bulb and corpus spongiosum
Within the erectile tissue, these arteries branch into smaller vessels called helicine arteries, which play a crucial role in the erection process.
Nervous System Components
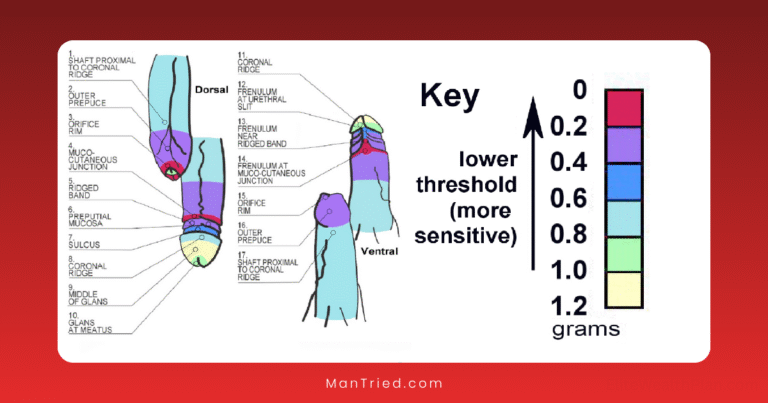
The penis receives innervation from both the autonomic (involuntary) and somatic (voluntary) nervous systems:
- Pudendal nerve: Provides sensory information and controls voluntary muscles
- Cavernous nerves: Part of the autonomic nervous system, these nerves regulate blood flow
- Sympathetic pathways: Originate from thoracolumbar segments (T11-L2) of the spinal cord
- Parasympathetic pathways: Originate from sacral segments (S2-S4) of the spinal cord
The Vascular Mechanism: A Matter of Blood Flow
At its core, an erection is a vascular event—a carefully orchestrated change in blood flow that transforms the penis from flaccid to erect.
The Flaccid State: Active Constriction
Contrary to what many might assume, the flaccid state of the penis is actually an active process, not a passive one. In this state:
- Smooth muscles in the penile arteries and erectile tissues are contracted
- Helicine arteries are narrowed, limiting blood flow
- Blood oxygen levels in the penis are relatively low (approximately 35 mmHg)
- Blood flows in and out at equal rates, maintaining the flaccid state
As PMC explains, “In the flaccid state, smooth muscles are tonically contracted, allowing minimal arterial flow.”
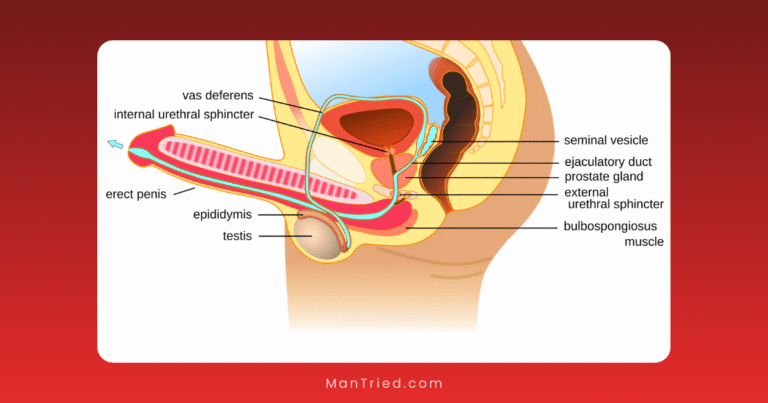
The Erection Sequence: A Five-Step Process
When sexual stimulation occurs, a cascade of vascular events follows:
- Arterial Dilation: The smooth muscles in penile arteries relax, increasing blood flow to the penis.
- Sinusoidal Filling: Blood fills the spaces (sinusoids) within the corpora cavernosa, causing them to expand.
- Compression of Venous Outflow: As the erectile tissues expand, they compress the veins against the tunica albuginea (the tough fibrous covering of the corpora cavernosa), reducing blood outflow.
- Pressure Increase: With more blood flowing in than out, pressure within the corpora cavernosa increases dramatically—from a resting pressure of about 10 mmHg to approximately 100 mmHg during full erection.
- Rigidity Development: The tunica albuginea has limited elasticity, so as the internal pressure increases, the penis becomes rigid rather than continuing to expand indefinitely.
During this process, blood oxygen levels in the penis rise from about 35 mmHg to approximately 90 mmHg, reflecting the increased arterial blood flow.
The Rigid-Erection Phase: Muscular Contribution
For maximum rigidity, particularly during penetration, additional muscular action comes into play:
- The ischiocavernosus muscles (which surround the base of the penis) contract
- This contraction further increases intracavernous pressure
- In some cases, pressure can reach levels as high as 200 mmHg during this phase
According to Cleveland Clinic, “The tunica albuginea, a membrane surrounding the corpora cavernosa, helps to maintain the erection by trapping blood.”
The Neurological Control: The Brain-Penis Connection
While the vascular changes are the mechanical means by which erections occur, the nervous system provides the control mechanisms that initiate and regulate the process.
Central Nervous System: Where Erections Begin
Several key brain regions are involved in processing sexual stimuli and initiating the erection response:
- Medial preoptic area (MPOA): A region of the hypothalamus that plays a crucial role in male sexual behavior
- Paraventricular nucleus (PVN): Another hypothalamic region involved in erection control
- Limbic system: Processes emotional and sensory inputs related to sexual arousal
- Cerebral cortex: Processes visual, auditory, olfactory, and imaginative sexual stimuli
Modern imaging studies using PET scans and fMRI have shown increased activity in these brain regions during sexual arousal, confirming their role in the erection process.
Types of Erections: Different Neural Pathways
Interestingly, erections can occur through different neural mechanisms:
- Psychogenic erections: Triggered by mental stimuli (fantasies, visual cues, etc.) processed in the brain and transmitted via descending pathways from the brain to the spinal cord and then to the penis.
- Reflexogenic erections: Occur in response to direct physical stimulation of the genitals, involving a spinal reflex arc that can function even in cases of complete spinal cord injury above the sacral level.
- Nocturnal erections: Occur during REM sleep, controlled by brainstem mechanisms. Most men experience 3-5 episodes of nocturnal erections per night, each lasting 20-40 minutes.
As PMC notes, “Erection can be categorized into three types: psychogenic, reflexogenic, and nocturnal, each involving different neural pathways.”
The Autonomic Balance: Sympathetic vs. Parasympathetic
The autonomic nervous system plays a critical role in erection control through two opposing branches:
- Sympathetic nervous system: Associated with the “fight or flight” response, it promotes flaccidity through the release of norepinephrine, which causes smooth muscle contraction in penile arteries.
- Parasympathetic nervous system: Associated with the “rest and digest” response, it promotes erection through the release of acetylcholine and nitric oxide, causing smooth muscle relaxation and increased blood flow.
During sexual arousal, parasympathetic activity increases while sympathetic activity decreases, shifting the balance toward erection. This explains why stress and anxiety (which activate the sympathetic nervous system) can inhibit erections.
The Biochemical Cascade: Molecular Messengers
At the molecular level, a sophisticated signaling cascade translates neural signals into the vascular changes necessary for erection.
The Nitric Oxide Pathway: The Master Regulator
Nitric oxide (NO) is the primary molecular mediator of penile erection. Here’s how the pathway works:
- Sexual stimulation causes the release of nitric oxide from nerve endings and endothelial cells in the penis.
- Nitric oxide diffuses into smooth muscle cells in the arterial walls and erectile tissues.
- Inside these cells, NO activates an enzyme called guanylyl cyclase, which converts guanosine triphosphate (GTP) into cyclic guanosine monophosphate (cGMP).
- cGMP acts as a second messenger, triggering a series of events that lead to decreased calcium levels in smooth muscle cells.
- With less calcium available, smooth muscle contraction is inhibited, resulting in relaxation and increased blood flow.
According to NCBI, “The mechanism of action involves the release of nitric oxide, which stimulates cGMP production, promoting relaxation of vascular smooth muscle.”
PDE5: The Erection Terminator
The erection process includes built-in mechanisms for its own termination:
- An enzyme called phosphodiesterase type 5 (PDE5) breaks down cGMP
- As cGMP levels fall, calcium returns to the smooth muscle cells
- Smooth muscles contract again, reducing blood flow
- The penis returns to its flaccid state
Understanding this mechanism led to the development of PDE5 inhibitors like sildenafil (Viagra), which block the action of PDE5, prolonging the effect of cGMP and enhancing erectile function.
Recent research from Nature indicates that “Nitric oxide activates molecular signaling pathways by increasing intracellular levels of cyclic guanosine monophosphate (cGMP),” and that “PDE5 inhibitors work to maintain cGMP levels, becoming ineffective in the absence of cGMP.”
The Hormonal Influence: Setting the Stage
While neural and vascular mechanisms are the immediate drivers of erection, hormones—particularly testosterone—play a crucial supporting role by creating the necessary conditions for these mechanisms to function properly.
Testosterone: The Foundation of Male Sexual Function
Testosterone affects erectile function in several ways:
- Libido regulation: Testosterone is essential for sexual desire, which initiates the erection process through psychogenic pathways.
- Nitric oxide production: Testosterone enhances the expression of nitric oxide synthase, the enzyme that produces NO.
- Penile tissue maintenance: Testosterone supports the health of erectile tissues and maintains their responsiveness to sexual stimulation.
- Neural sensitivity: Adequate testosterone levels are necessary for proper functioning of the neural pathways involved in erection.
Studies have shown that men with low testosterone levels may experience erectile dysfunction, and testosterone replacement therapy can improve erectile function in these cases—though it’s not effective for ED with other causes.
Other Hormonal Players
While testosterone is the primary hormonal factor in erections, other hormones also play roles:
- Prolactin: Elevated levels can suppress testosterone and inhibit erectile function.
- Thyroid hormones: Both hypothyroidism and hyperthyroidism can contribute to erectile dysfunction.
- Cortisol: This stress hormone can interfere with erectile function when chronically elevated.
- Oxytocin: Released during sexual arousal, it may enhance erection and ejaculation.
When Things Go Wrong: Erectile Dysfunction
Understanding the complex physiology of erections helps explain why so many different factors can lead to erectile dysfunction (ED).
The Scale of the Issue
Erectile dysfunction is remarkably common:
- According to Hopkins Medicine, “In 1995, over 152 million men worldwide experienced ED; this number is predicted to rise to approximately 322 million by 2025.”
- The Massachusetts Male Aging Study found a total prevalence of ED of 52% among men aged 40-70 years.
- ED prevalence increases with age, affecting approximately 40% of men at age 40 and nearly 70% of men at age 70.
Vascular Causes of ED
Given the central role of blood flow in erections, it’s not surprising that vascular issues are the most common cause of ED:
- Atherosclerosis: Plaque buildup in arteries restricts blood flow to the penis.
- Hypertension: Can damage blood vessels and reduce blood flow.
- Diabetes: Causes both vascular damage and nerve damage.
- Venous leakage: Inability to trap blood in the penis due to venous dysfunction.
Neurological Causes of ED
Disruptions to the neural pathways controlling erection can also lead to ED:
- Spinal cord injury: Can interrupt the nerve signals between the brain and penis.
- Multiple sclerosis: Damages nerve pathways throughout the body.
- Parkinson’s disease: Affects both central and peripheral neural function.
- Surgical damage: Particularly following prostate surgery, which can damage the cavernous nerves.
Hormonal Causes of ED
Hormonal imbalances, particularly involving testosterone, can contribute to ED:
- Hypogonadism: Low testosterone production.
- Thyroid disorders: Both over- and under-active thyroid can affect erectile function.
- Hyperprolactinemia: Elevated prolactin levels suppress testosterone.
Medication-Induced ED
Many medications can interfere with the erection process:
- Antihypertensives: Particularly beta-blockers and diuretics.
- Antidepressants: Especially selective serotonin reuptake inhibitors (SSRIs).
- Antiandrogens: Used in prostate cancer treatment.
- Opioids: Can suppress testosterone production.
Psychological Factors
The mind-body connection is particularly evident in erectile function:
- Performance anxiety: Creates a cycle of fear and failure.
- Depression: Affects both desire and physical response.
- Stress: Activates the sympathetic nervous system, inhibiting erection.
- Relationship issues: Can interfere with the arousal necessary to initiate erections.
Modern Treatments: Targeting Specific Mechanisms
Understanding the physiological mechanisms of erection has led to targeted treatments for erectile dysfunction:
PDE5 Inhibitors: The First-Line Treatment
These medications, including sildenafil (Viagra), tadalafil (Cialis), vardenafil (Levitra), and avanafil (Stendra), work by targeting a specific step in the biochemical cascade:
- They inhibit the enzyme phosphodiesterase type 5 (PDE5)
- This prevents the breakdown of cGMP in erectile tissues
- Higher cGMP levels enhance and prolong smooth muscle relaxation
- The result is improved blood flow and better erectile function
According to NCBI, “PDE5 inhibitors are now the first-line treatment for erectile dysfunction (ED)” with “an estimated 320 million individuals projected to experience erectile dysfunction by 2025.”
It’s important to note that PDE5 inhibitors require sexual stimulation to work—they enhance the natural process rather than triggering erections independently. This is because they don’t create cGMP; they only prevent its breakdown after it’s naturally produced in response to sexual arousal.
Recent research from MDPI indicates that beyond their effects on erections, “PDE5 inhibitors may exert anti-inflammatory effects by reducing vascular inflammation and enhancing cGMP signaling,” suggesting potential additional health benefits.
Addressing Hormonal Factors: Testosterone Replacement
For men with low testosterone levels (hypogonadism), testosterone replacement therapy may improve erectile function by:
- Increasing sexual desire, which initiates the erection process
- Enhancing nitric oxide production
- Improving the health and responsiveness of erectile tissues
Testosterone can be administered through injections, patches, gels, or pellets implanted under the skin. However, it’s only effective for ED caused by low testosterone and won’t help when other mechanisms are responsible.
Targeting Vascular Mechanisms: Alprostadil
For men who don’t respond to PDE5 inhibitors, alprostadil provides an alternative approach:
- Alprostadil is a synthetic version of prostaglandin E1, a natural vasodilator
- It can be administered as an injection directly into the penis (intracavernosal injection)
- It can also be used as a urethral suppository (intraurethral application)
- It causes smooth muscle relaxation and increased blood flow independent of the NO-cGMP pathway
This treatment bypasses the need for neural signals and nitric oxide release, making it effective even for men with neurological causes of ED.
Vacuum Erection Devices: Mechanical Assistance
These devices work purely on physical principles to create an erection:
- A cylinder is placed over the penis
- Air is pumped out, creating a vacuum
- The vacuum draws blood into the penis
- A constriction ring placed at the base of the penis traps the blood
- This maintains the erection for up to 30 minutes
This approach bypasses both neural and vascular mechanisms, making it suitable for men with various types of ED.
Penile Implants: The Surgical Solution
For men who don’t respond to other treatments, penile implants provide a permanent solution:
- Inflatable implants: Cylinders implanted in the penis can be filled with fluid from a reservoir to create an erection
- Semi-rigid implants: Malleable rods that allow the penis to be positioned for intercourse
According to Hopkins Medicine, penile implants have “a low infection rate of less than 2%” and high satisfaction rates among patients and partners.
Emerging Treatments: Next-Generation Approaches
Research continues to develop new approaches based on our understanding of erection physiology:
- Low-intensity extracorporeal shockwave therapy (LI-ESWT): Aims to improve penile blood flow by stimulating the growth of new blood vessels
- Platelet-rich plasma (PRP) injections: Uses growth factors from the patient’s own blood to potentially regenerate erectile tissues
- Stem cell therapy: Experimental approach aiming to regenerate damaged erectile tissues
- Nitric oxide microparticle delivery: As described in Nature, combining “nitric oxide microparticle delivery (NO-MP) with FDA-approved PDE5 inhibitors” shows promise for improving erectile responses in experimental models
The Mind-Body Connection: Psychological Aspects of Erections
While we’ve focused on the physiological mechanisms of erection, the psychological dimension is equally important and intricately connected to these physical processes.
The Psychogenic Pathway: Thoughts to Erection
The ability to achieve an erection through mental stimulation alone—without physical touch—demonstrates the power of the brain-penis connection:
- Visual, auditory, olfactory stimuli, or sexual thoughts activate brain regions associated with sexual arousal
- These brain regions send signals via the spinal cord to the genital region
- The signals trigger the same vascular changes as physical stimulation
This pathway explains why psychological factors can so profoundly influence erectile function.
Performance Anxiety: The Vicious Cycle
One of the most common psychological factors affecting erections is performance anxiety:
- Concern about erectile performance activates the sympathetic nervous system
- Sympathetic activation promotes the flaccid state through norepinephrine release
- This makes erection more difficult, confirming the original anxiety
- The cycle reinforces itself with each unsuccessful attempt
Breaking this cycle often requires addressing both the psychological anxiety and, temporarily, the physiological response through medications like PDE5 inhibitors.
The Impact of Stress and Emotions
The autonomic nervous system—which controls erections—is highly responsive to emotional states:
- Stress: Activates the sympathetic “fight or flight” response, inhibiting erection
- Anxiety: Similar to stress, shifts autonomic balance toward sympathetic dominance
- Depression: Affects both desire (libido) and the neurochemical environment needed for erections
- Anger: Can either inhibit or, in some cases, facilitate erections depending on context
- Relaxation: Promotes parasympathetic dominance, facilitating erections
This connection explains why relaxation techniques, mindfulness, and stress management can improve erectile function in some men.
Lifestyle Factors: Protecting Erectile Function
The complex physiology of erections is influenced by overall health and lifestyle choices, creating opportunities to protect and enhance erectile function naturally.
Cardiovascular Health: The Vascular Connection
Given that erections are primarily vascular events, cardiovascular health is directly linked to erectile function:
- Exercise: Regular physical activity improves endothelial function, enhancing nitric oxide production and blood vessel health
- Diet: Mediterranean-style diets rich in fruits, vegetables, whole grains, and healthy fats support vascular health
- Weight management: Obesity is associated with reduced testosterone and increased inflammatory markers that impair erectile function
- Blood pressure control: Hypertension damages blood vessels, including those supplying the penis
- Cholesterol management: High cholesterol contributes to atherosclerosis, restricting penile blood flow
Habits That Impact Erectile Function
Several common habits directly affect the physiological mechanisms of erection:
- Smoking: Damages blood vessels and reduces nitric oxide availability
- Excessive alcohol: Interferes with neural signaling and can suppress testosterone production
- Recreational drugs: Many drugs, including marijuana, cocaine, and opioids, can impair erectile function through various mechanisms
- Sleep deprivation: Reduces testosterone levels and increases stress hormones
- Sedentary lifestyle: Contributes to vascular disease and reduces testosterone
Protecting Neural Pathways
The neurological aspects of erection can also be affected by lifestyle:
- Diabetes management: Poor glucose control damages nerves, including those controlling erection
- Avoiding toxin exposure: Some environmental toxins and heavy metals can damage nerves
- Preventing injury: Protecting the spine and pelvic region from injury preserves neural pathways
- Pelvic floor exercises: Strengthen the muscles involved in erection and ejaculation
Beyond Pathology: Optimizing Erectile Function
Most discussions of erectile physiology focus on dysfunction and treatment, but understanding these mechanisms also offers insights for optimizing normal function.
Natural Enhancers of the Erection Process
Several nutrients and compounds may support the physiological mechanisms of erection:
- L-arginine and L-citrulline: Amino acids that serve as precursors for nitric oxide production
- Antioxidants: Protect nitric oxide from degradation and support blood vessel health
- Zinc: Essential for testosterone production
- Vitamin D: Associated with testosterone levels and overall sexual function
According to PMC, “Other substances that increase NO production include alprostadil, papaverine, L-arginine, L-citrulline, resveratrol, and α-lipoic acid.”
Training the System: Physiological Conditioning
Like other physiological systems, the erectile mechanism may respond to appropriate “training”:
- Kegel exercises: Strengthen the ischiocavernosus and bulbospongiosus muscles that assist in erection
- Regular sexual activity: Maintains healthy blood flow and tissue oxygenation
- Mindfulness practices: Improve the mind-body connection and reduce performance anxiety
- Cardiovascular exercise: Enhances overall vascular health, including penile blood flow
Conclusion: A Marvel of Physiological Integration
The erection process stands as a remarkable example of physiological integration—where vascular, neurological, and hormonal systems work in precise coordination to achieve a specific function. This complexity explains both why so many factors can disrupt erectile function and why a multifaceted approach is often needed to address dysfunction.
Understanding these mechanisms empowers men to:
- Recognize how lifestyle choices affect erectile function
- Understand the rationale behind various treatments
- Communicate more effectively with healthcare providers
- Make informed decisions about sexual health
As research continues to deepen our understanding of erectile physiology, new approaches to both treating dysfunction and optimizing function will likely emerge, further enhancing men’s sexual health across the lifespan.
Have questions about erectile physiology or sexual health? Share them in the comments below.