Male Sexual Anatomy: The Parts Nobody Talks About
When it comes to male sexual anatomy, most conversations begin and end with the penis. It’s as if men’s bodies consist of one solitary organ, with everything else relegated to supporting roles or ignored entirely. This limited perspective not only creates gaps in knowledge but can also lead to missed opportunities for pleasure, inadequate healthcare, and unnecessary shame.
The truth is that male sexual anatomy is complex, nuanced, and worthy of more comprehensive understanding. This guide explores the lesser-discussed aspects of male sexual anatomy—the parts that rarely make it into locker room conversations or even doctor’s visits, but which play crucial roles in sexual health, function, and pleasure.
Beyond the Basics: A More Complete Picture
Most men are familiar with the basic external anatomy—penis, scrotum, and testicles. But even these familiar parts have aspects that aren’t widely discussed.
The Penis: More Than Meets the Eye
While the penis gets plenty of attention, certain aspects of its anatomy remain surprisingly under-discussed:
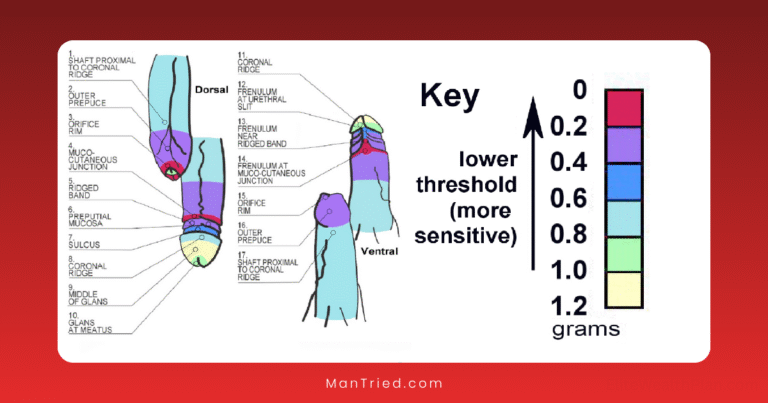
The Frenulum: The Male Sweet Spot
The frenulum is a highly sensitive V-shaped area on the underside of the penis where the glans (head) meets the shaft. According to MensXP, this area is “often compared to the sensitivity of the clitoris” and is considered “the main trigger for orgasms in men” for many.
This band of tissue contains a concentration of nerve endings that make it particularly responsive to light touch, pressure, or vibration. For some men, stimulation of just the frenulum alone can lead to orgasm.
What you should know: The frenulum can be shorter in some men, a condition called frenulum breve, which can cause discomfort during erection or sex. Circumcision sometimes removes part or all of the frenulum, which can affect sensitivity.
The Corpora Cavernosa: The Erectile Chambers
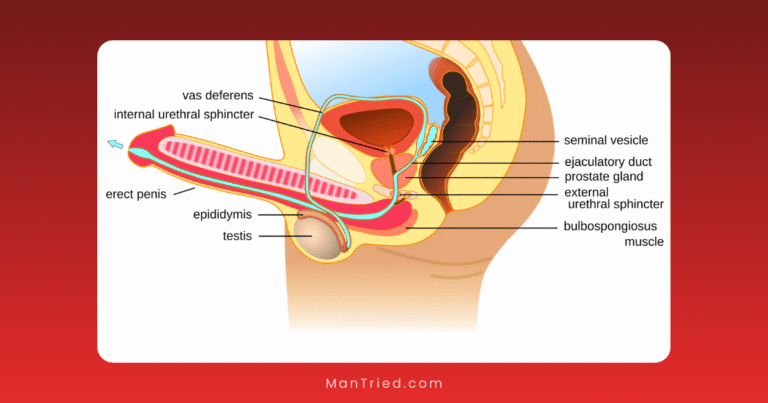
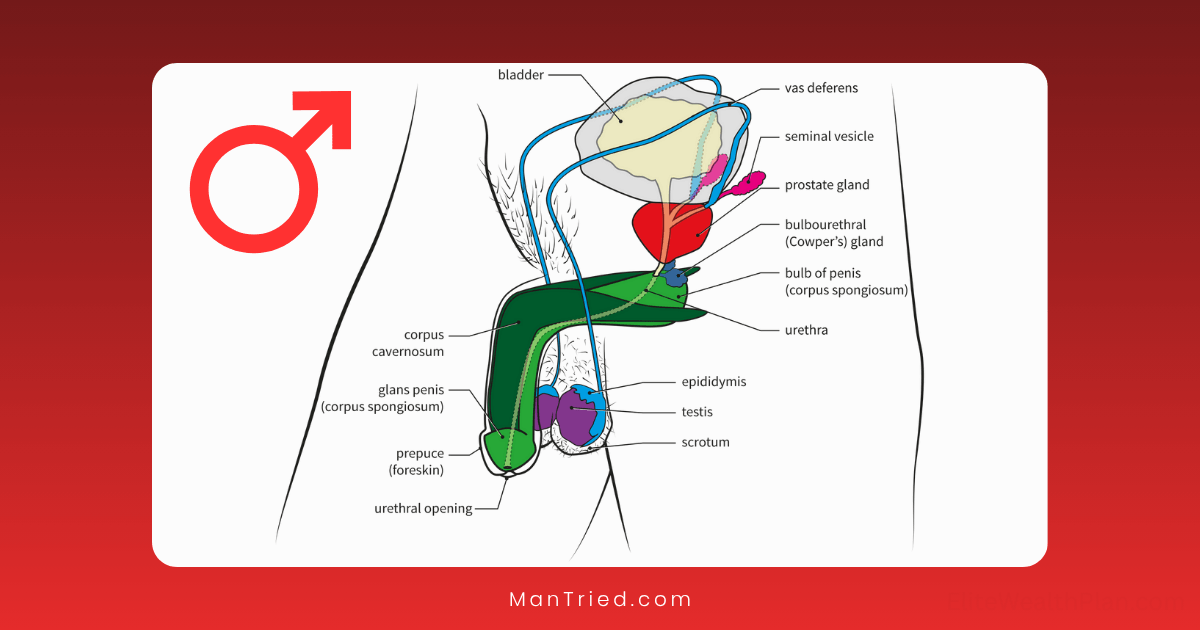
Inside the penis are three chambers of spongy tissue. The two larger ones on top, called the corpora cavernosa, and a smaller one underneath, the corpus spongiosum. These chambers fill with blood during arousal, creating an erection.
According to Cleveland Clinic, “The body of the penis contains three internal chambers: two corpora cavernosa and one corpus spongiosum.”
What you should know: The health of these chambers and their blood vessels directly affects erectile function. Conditions like cardiovascular disease can impact blood flow to these chambers long before more obvious symptoms appear elsewhere in the body, making erectile changes an important early warning sign worth discussing with healthcare providers.
The Perineum: The Forgotten Pleasure Zone
The perineum is the area of skin between the scrotum and the anus. Despite being packed with nerve endings and providing access to deeper structures, it rarely gets mentioned in discussions about male sexuality.
Healthline describes it as “the area of skin between the scrotum and anus” that “can also be stimulated to indirectly affect the prostate.”
This region contains the bulb of the penis—the internal portion of the penis that extends into the body—and is rich with nerve endings. Pressure or massage here can stimulate the internal structures of the penis as well as indirectly stimulate the prostate.
What you should know: The perineum hardens during arousal as the bulb of the penis fills with blood. This area is also vulnerable to injury during certain activities like cycling, and discomfort here can indicate conditions like prostatitis or pelvic floor dysfunction.
The Prostate: The “Male G-Spot”
Perhaps the most significant yet least discussed aspect of male sexual anatomy is the prostate gland. Often referred to as the “male G-spot” or “P-spot,” this walnut-sized gland is located internally, about 2 inches inside the rectum toward the front of the body.
Medical News Today explains that the prostate is “a walnut-sized gland located between the base of the penis and the rectum” and consists of “three zones: peripheral zone (70% of the prostate), central zone, and transitional zone.”
The prostate serves several important functions:
- Produces prostatic fluid, a component of semen
- Contains muscles that help expel semen during ejaculation
- Houses nerves that play a role in sexual pleasure
What you should know: The prostate contains numerous nerve endings and, when stimulated, can produce intense sensations and powerful orgasms that feel different from penile orgasms. Some men report whole-body orgasms from prostate stimulation that don’t necessarily involve ejaculation.
According to Anoeses, “The prostate is rich in nerve endings and is deeply connected to the body’s orgasmic system” and “stimulating the prostate can trigger powerful, full-body sensations, especially when combined with external touch.”
Internal Structures: The Hidden System
Beyond these more accessible parts lie several internal structures that play crucial roles in sexual function but rarely enter public conversation.
The Bulbourethral Glands: The Pre-Show Producers
Also known as Cowper’s glands, these pea-sized glands located just below the prostate produce pre-ejaculatory fluid, or “pre-cum.” This clear fluid serves several important functions:
- Neutralizes acidity in the urethra to create a more hospitable environment for sperm
- Provides some lubrication during sexual activity
- May contain some sperm cells, though in smaller numbers than ejaculate
Planned Parenthood notes that “Cowper’s glands produce pre-ejaculate fluid that prepares the urethra for ejaculation.”
What you should know: While pre-ejaculatory fluid contains fewer sperm than ejaculate, it can still contain enough to cause pregnancy, making withdrawal an unreliable birth control method. The amount of pre-ejaculatory fluid varies significantly between individuals.
The Cremaster Muscle: The Temperature Regulator
This fascinating muscle receives little attention despite its important role. The cremaster muscle surrounds the spermatic cord and testicles and controls their position relative to the body.
Planned Parenthood explains that “The cremaster muscle moves the scrotum and testicles closer to the body in response to cold, arousal, or touch.”
What you should know: The cremaster reflex—the automatic raising of the testicles in response to cold, touch, or arousal—is normal and serves to regulate testicular temperature for optimal sperm production. Excessive cremasteric reflex, where the testicles retract too frequently or strongly, can sometimes indicate underlying health issues.
The Epididymis: The Maturation Chamber
The epididymis is a tightly coiled tube attached to the back of each testicle. Despite its crucial role in sperm development, it’s rarely mentioned outside medical contexts.
According to Hopkins Medicine, “The epididymis is a long tube near each testicle that moves sperm from the testicles.”
This structure:
- Stores sperm produced in the testicles
- Allows sperm to mature and develop motility
- Connects to the vas deferens, which carries sperm toward the urethra
What you should know: The epididymis can become inflamed or infected (epididymitis), causing pain and swelling. This condition is often mistaken for testicular problems and requires medical attention. The epididymis is also the site of vasectomy procedures, where the connecting tube is cut or blocked.
Nerve Pathways: The Pleasure Network
The physical structures of male sexual anatomy are only part of the story. Equally important is the network of nerves that transmit sensation and control function.
The Pudendal Nerve: The Main Sensory Highway
The pudendal nerve is the primary nerve responsible for carrying sensations from the genitals to the brain. This nerve has several branches that innervate different areas:
- The dorsal nerve of the penis, providing sensation to the penis
- The perineal nerve, serving the perineum, scrotum, and part of the anus
- The inferior rectal nerve, providing sensation to the anal region
What you should know: Damage to the pudendal nerve from prolonged sitting, cycling, or certain medical conditions can lead to decreased sensation or even chronic pain. Proper bike seats and good posture can help protect this crucial nerve.
The Pelvic Floor Muscles: The Unsung Support System
The pelvic floor is a group of muscles that form a hammock-like structure at the bottom of the pelvis. These muscles support the bladder, rectum, and other pelvic organs, and play crucial roles in sexual function:
- Help maintain erections
- Contract during orgasm
- Control ejaculation timing
- Support the prostate and other internal structures
What you should know: Pelvic floor dysfunction can contribute to erectile difficulties, premature ejaculation, or pain during sexual activity. Pelvic floor physical therapy and exercises like Kegels can help address these issues but are rarely discussed in men’s health conversations.
Psychological Dimensions: The Mind-Body Connection
No discussion of sexual anatomy would be complete without acknowledging the powerful role of the mind. The brain is, after all, the largest and most important sexual organ.
The Brain’s Role in Arousal
Sexual arousal begins in the brain, with the limbic system (particularly the amygdala and hippocampus) playing key roles in processing sexual stimuli and triggering physical responses. The hypothalamus then signals the release of hormones that initiate the physiological aspects of arousal.
What you should know: Psychological factors like stress, anxiety, or negative body image can interrupt these neural pathways, affecting physical arousal regardless of stimulation. Understanding this connection can help address issues that might otherwise be mistakenly attributed to physical dysfunction.
Body Image and Male Anatomy
Men’s relationships with their bodies, particularly their genitals, can significantly impact sexual confidence and function. Concerns about penis size, appearance, or performance are common but rarely discussed openly.
What you should know: Research consistently shows that most men overestimate what’s “average” and underestimate their own measurements. According to Cleveland Clinic, “The average penis size is approximately 3.5 inches (8.9 cm) when flaccid and a little more than 5 inches (13 cm) when erect.”
Cultural and Personal Perspectives
How we understand and talk about male anatomy varies significantly across cultures, generations, and individual experiences.
Cultural Differences in Anatomical Understanding
Different cultures have varying levels of openness about male anatomy and different traditional understandings of how these parts function. Some cultures have long traditions of practices focused on less-discussed aspects of male anatomy, such as prostate massage in certain traditional medicine systems.
The Language Gap
One challenge in discussing male anatomy is the lack of comfortable, accurate vocabulary. Terms tend to be either clinical and sterile or crude and potentially offensive. This language gap makes conversations about these body parts difficult, whether in educational, medical, or intimate contexts.
Practical Applications: Knowledge in Action
Understanding the less-discussed aspects of male sexual anatomy has practical benefits for health, pleasure, and communication.
Health Awareness and Early Detection
Knowledge of complete male anatomy helps with:
- Recognizing potential health issues early
- Understanding what’s normal versus what needs medical attention
- Having more productive conversations with healthcare providers
- Making informed decisions about procedures like circumcision or vasectomy
Enhancing Pleasure and Connection
A more comprehensive understanding of male anatomy can lead to:
- Exploration of new sources of pleasure beyond the conventional
- Better communication with partners about preferences and sensations
- Reduced performance pressure by expanding the definition of male sexuality
- More satisfying solo sexual experiences through greater self-knowledge
Improving Communication
Better anatomical knowledge enables:
- More precise descriptions of sensations or concerns to partners and healthcare providers
- Reduced embarrassment when discussing sexual health issues
- More nuanced understanding of how various conditions or medications might affect sexual function
- Greater comfort in educating others, including children, about bodies in age-appropriate ways
Conclusion: Breaking the Silence
The limited public conversation about male sexual anatomy does a disservice to everyone. By expanding our understanding beyond the basics, we create opportunities for better health outcomes, more satisfying intimate experiences, and more honest communication.
The parts nobody talks about deserve attention—not just in medical textbooks or behind closed doors, but in our broader cultural conversation about bodies and sexuality. By normalizing discussions of complete male anatomy, we can help reduce shame, increase knowledge, and promote both physical and emotional well-being.
After all, knowledge of our bodies isn’t just academic—it’s fundamental to how we experience ourselves and connect with others. And that’s something worth talking about.
Have you learned something new about male anatomy from this article? What aspects of this topic do you think deserve more attention in public health education? Share your thoughts in the comments below.