Ejaculation Mechanics: The Complete Physiological Process Explained
Ejaculation is often understood simply as the expulsion of semen from the penis during sexual climax. However, beneath this seemingly straightforward event lies an intricate symphony of neurological signals, hormonal influences, and precisely coordinated muscular contractions. This article dives deep into the fascinating mechanics of ejaculation, breaking down the complex physiological process into understandable components.
The Two-Phase Process
According to research published in the Journal of Sexual Medicine, ejaculation consists of two distinct yet seamlessly integrated phases:
- Emission Phase: The preparation and collection of reproductive fluids
- Expulsion Phase: The forceful ejection of these fluids through the urethra
Let’s explore each phase in detail to understand the remarkable orchestration of biological events that occur.
The Emission Phase: Setting the Stage
The emission phase begins with sexual arousal and continues until just before the moment of ejaculation. During this phase, several key events occur simultaneously:
Sperm Mobilization
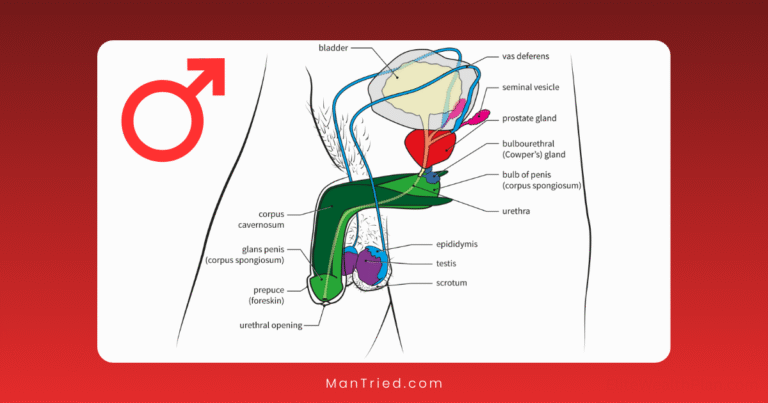
Stored in the epididymis (a coiled tube attached to each testicle), sperm cells are inactive until sexual arousal triggers their movement. According to Britannica Science, muscular contractions in the epididymis and vas deferens (sperm ducts) propel sperm toward the ampulla, a widened portion of the vas deferens near the prostate.
Glandular Secretions
Multiple accessory glands activate to contribute their specialized fluids:
- Prostate Gland: Produces a thin, milky fluid that constitutes about 30% of semen volume. This alkaline fluid contains enzymes like prostate-specific antigen (PSA), which helps liquefy semen after ejaculation, and zinc, which protects sperm DNA.
- Seminal Vesicles: These gland-like pouches contribute approximately 70% of seminal fluid volume. Their secretions contain fructose (energy for sperm), prostaglandins (to suppress the female immune response to sperm), and proteins that give semen its viscous consistency.
- Bulbourethral Glands (Cowper’s Glands): Release a clear pre-ejaculatory fluid that neutralizes any acidic residue in the urethra from urine and lubricates the urethra for sperm passage.
Research from the National Institutes of Health indicates that these secretions are produced in a specific sequence, creating a layered composition in the final ejaculate that optimizes sperm survival and function.
Bladder Neck Closure
A critical event during emission is the closure of the bladder neck (internal sphincter). This prevents retrograde ejaculation—the backflow of semen into the bladder—and ensures forward propulsion of seminal fluid.
According to a 2023 study in European Urology, this process is controlled by alpha-adrenergic receptors responding to norepinephrine released from sympathetic nerve fibers.
The Neural Control of Emission
The emission phase is primarily governed by the sympathetic nervous system—the same system responsible for our “fight or flight” response. Key neural components include:
- Thoracolumbar Spinal Cord (T10-L2): Houses the sympathetic neurons that control emission
- Hypogastric Nerve: Transmits signals from the spinal cord to the reproductive organs
- Superior Hypogastric Plexus: A network of nerves that coordinates the sympathetic input
Dr. Marcel Waldinger, a renowned researcher in sexual medicine, explains: “The sympathetic nervous system activation during emission explains why intense excitement or anxiety can sometimes trigger premature ejaculation—the system is already in a heightened state of arousal.”
The Expulsion Phase: The Moment of Release
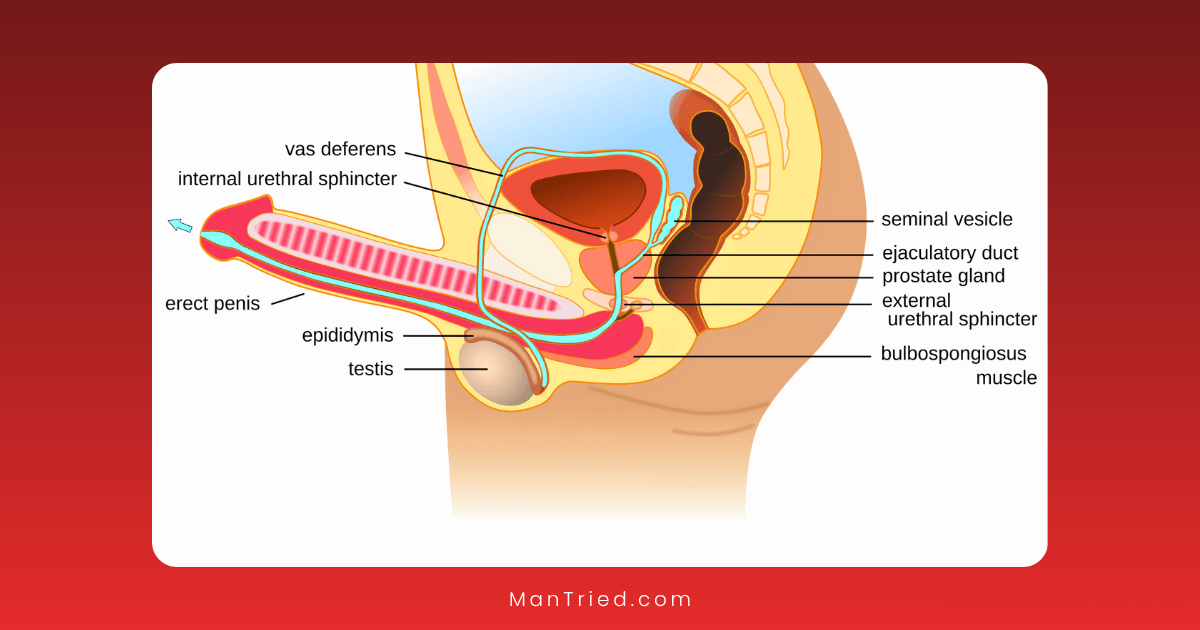
Once emission is complete and seminal fluid has collected in the bulbar urethra, the expulsion phase begins. This phase represents what most people recognize as ejaculation—the forceful expulsion of semen from the penis.
Muscular Contractions
The expulsion phase involves rhythmic contractions of several muscle groups:
- Bulbocavernosus Muscle: Wraps around the bulb of the penis and contracts rhythmically (typically 3-15 contractions) to propel semen forward. According to research published in The Journal of Urology, these contractions occur at approximately 0.8-second intervals during orgasm.
- Ischiocavernosus Muscles: Contract to help maintain erection during ejaculation and contribute to the expulsive force.
- Pelvic Floor Muscles: Provide additional force through coordinated contractions.
- Urethral Smooth Muscle: Contracts in waves to move semen along the urethra.
Research from the American Physiological Society has measured the pressure generated during these contractions, finding that the average intra-urethral pressure during ejaculation can reach 200-500 cm H₂O—enough force to propel semen up to 30 centimeters in some cases.
The Role of the External Urethral Sphincter
During expulsion, the external urethral sphincter (a muscle that normally keeps the urethra closed) relaxes to allow the passage of semen. This relaxation is coordinated with the contraction of other muscles to ensure efficient expulsion.
Neural Control of Expulsion
Unlike emission, the expulsion phase involves a complex interplay between sympathetic, parasympathetic, and somatic nervous systems:
- Sacral Spinal Cord (S2-S4): Contains the somatic neurons controlling the pelvic floor muscles
- Pudendal Nerve: Transmits signals to the bulbocavernosus and other pelvic floor muscles
- Spinal Ejaculation Generator: A specialized group of neurons in the lumbar spinal cord that coordinates the entire ejaculatory process
Recent research published in Nature Reviews Urology has identified specific lumbar spinothalamic (LSt) cells in the spinal ejaculation generator that are essential for coordinating ejaculation. These cells integrate sensory input from the genitals with descending signals from the brain to trigger the ejaculatory reflex at the appropriate time.
The Brain’s Role in Ejaculation
While ejaculation is primarily a spinal reflex, the brain plays crucial roles in both initiating and modulating the process:
Brain Regions Involved
Several brain regions are activated during ejaculation, as revealed by functional MRI studies published in The Journal of Sexual Medicine:
- Paraventricular Nucleus of the Hypothalamus: Releases oxytocin, which enhances contractile activity
- Medial Preoptic Area: Integrates sensory information and sexual motivation
- Nucleus Paragigantocellularis: Provides inhibitory control over ejaculation
- Cerebral Cortex: Processes sensory information and contributes to the conscious experience
Neurotransmitter Regulation
The timing and intensity of ejaculation are regulated by a delicate balance of neurotransmitters:
- Dopamine: Promotes ejaculation through D2-like receptors
- Serotonin: Generally inhibits ejaculation, particularly through 5-HT1A and 5-HT2C receptors
- Norepinephrine: Facilitates seminal emission and muscle contractions
- Oxytocin: Enhances contractile activity during expulsion
- Nitric Oxide: Plays a modulatory role, generally inhibiting ejaculation
This neurochemical balance explains why certain medications, particularly selective serotonin reuptake inhibitors (SSRIs), can delay ejaculation—a side effect sometimes utilized in treating premature ejaculation.
The Composition and Journey of Ejaculate
The average ejaculate volume ranges from 2-5 milliliters, though this can vary based on factors like age, health status, and time since last ejaculation.
According to research from the World Health Organization, a typical ejaculate contains:
- Sperm cells (50-150 million per milliliter)
- Seminal vesicle secretions (70% of volume)
- Prostatic fluid (25-30% of volume)
- Bulbourethral gland secretions (< 5% of volume)
- Trace amounts of epithelial cells and immunological cells
These components are not thoroughly mixed but rather layered in the ejaculate, with the first portion containing more prostatic fluid and the later portions containing more seminal vesicle fluid and sperm.
The Refractory Period: The Aftermath
Following ejaculation, men enter a refractory period during which another ejaculation cannot occur. According to research published in the International Journal of Impotence Research, this period varies significantly between individuals:
- Young men: Minutes to an hour
- Middle-aged men: 30 minutes to several hours
- Older men: 12-24 hours or longer
The physiological basis for this refractory period involves several mechanisms:
- Prolactin Release: Ejaculation triggers a surge in prolactin, which inhibits sexual arousal
- Autonomic Nervous System Reset: The sympathetic system requires time to recover
- Opioid Release: Endogenous opioids released during orgasm suppress further sexual response
- Serotonin Effects: Post-ejaculatory increases in serotonin inhibit further sexual activity
Factors Affecting Ejaculation
Multiple factors can influence the ejaculatory process:
Physiological Factors
- Age: Older men typically experience decreased ejaculate volume and force
- Hydration Status: Dehydration can reduce seminal fluid volume
- Frequency of Ejaculation: More frequent ejaculation typically results in lower volume
- Health Conditions: Diabetes, hypertension, and neurological disorders can affect ejaculatory function
- Medications: Alpha-blockers, antidepressants, and antipsychotics can impact ejaculation
Psychological Factors
- Arousal Level: Higher arousal typically leads to more forceful ejaculation
- Anxiety: Can lead to premature ejaculation or, conversely, delayed ejaculation
- Stress: Activates the sympathetic nervous system, potentially affecting timing
- Focus and Attention: Mindfulness during sexual activity can influence ejaculatory control
Common Ejaculatory Dysfunctions
Understanding the physiological process of ejaculation provides insight into various dysfunctions:
Premature Ejaculation
Affecting approximately 30% of men at some point, premature ejaculation involves ejaculation that occurs sooner than desired. Research from the International Society for Sexual Medicine suggests it often results from hypersensitivity of the ejaculatory reflex or imbalances in serotonin signaling.
Delayed Ejaculation
Characterized by significant delay or inability to achieve ejaculation despite adequate stimulation. According to the American Urological Association, this can result from neurological issues, hormonal imbalances, or psychological factors.
Retrograde Ejaculation
Occurs when semen enters the bladder rather than being expelled through the urethra, often due to dysfunction of the bladder neck closure mechanism. This is common after certain prostate surgeries or in men with diabetic neuropathy.
Anejaculation
The complete absence of ejaculation despite orgasm (dry orgasm) or the inability to reach orgasm. This can result from nerve damage, certain medications, or psychological issues.
Modern Research and Future Directions
Recent advances in understanding ejaculation mechanics include:
- Optogenetic Studies: Using light-activated proteins to control specific neurons involved in ejaculation
- Neuromodulation Techniques: Targeted electrical stimulation to treat ejaculatory dysfunctions
- Pharmacological Developments: More selective drugs that target specific receptors involved in ejaculation
- Imaging Technologies: Advanced MRI techniques to visualize brain activity during ejaculation in real-time
Dr. Emmanuele Jannini, a leading researcher in sexual medicine, notes: “We’re moving toward a more nuanced understanding of ejaculation that recognizes it not as a simple reflex but as a complex process involving multiple systems and capable of significant plasticity and learning.”
Conclusion: A Marvel of Physiological Coordination
Ejaculation represents one of the most complex and precisely coordinated physiological processes in the male body. From the careful preparation and collection of reproductive fluids to their forceful expulsion, the process involves intricate communication between the brain, spinal cord, autonomic nervous system, and multiple organ systems.
Understanding this remarkable process not only satisfies scientific curiosity but also provides the foundation for addressing the many issues that can affect this important aspect of male sexual function. As research continues to unravel the complexities of ejaculation, we can expect more effective treatments for ejaculatory dysfunctions and a deeper appreciation for this fundamental aspect of human reproduction.